by Moshood Isah
In recent times, the focus of conversations in digital health forums has increasingly centered around optimizing and integrating existing solutions to enhance surveillance, preparedness, and impact. This is not unconnected to the fact that the world and especially the African region has endured a series of public health emergencies and disease outbreaks which required urgent responses.
The World Health Organization also echoed that the 21st century health challenges like the pandemic have further accelerated the use of digital health interventions, including hotlines, online assistance, mobile phone applications and many more. These innovations have shown potential in reducing the interruption of Non Communicable Diseases (NCDs) and mental health services, making it necessary to continue scaling up digital health technology.
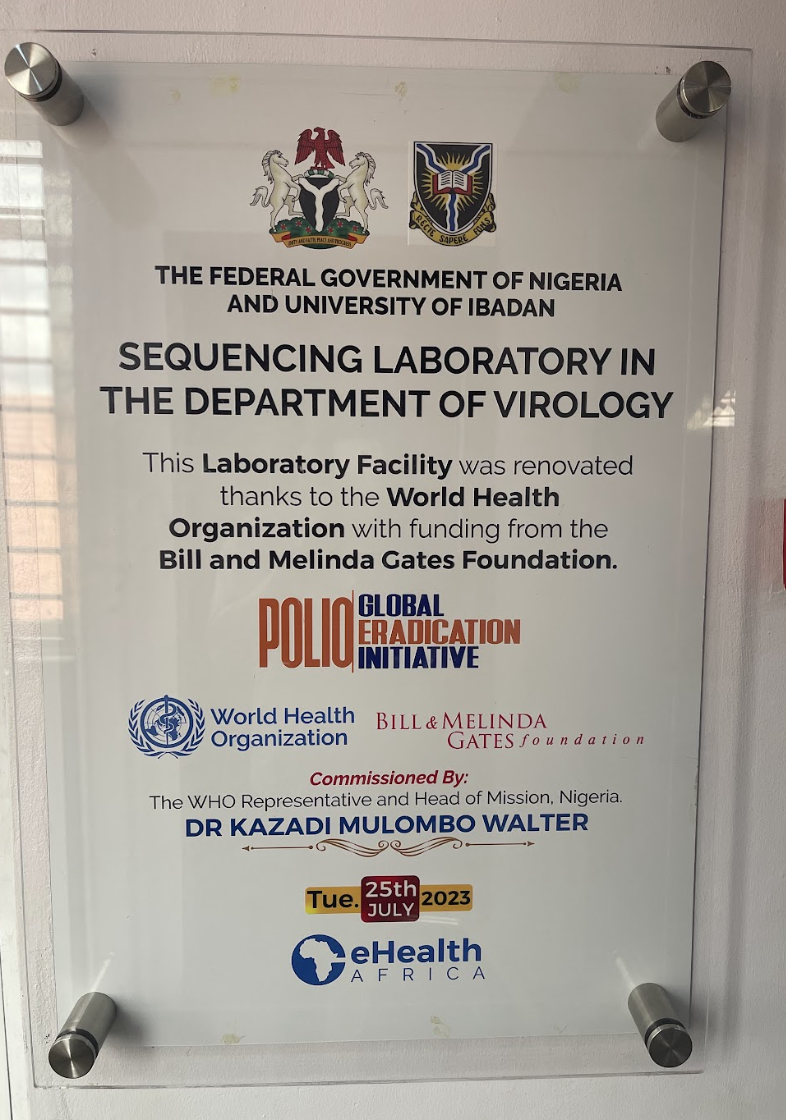
Health stakeholders have consistently taken intentional steps to stimulate ideas and expand advocacy to improve the impact of these solutions, especially when it comes to disease surveillance. One such conversation is the Insights Learning Forum (ILF 2024) hosted by eHealth Africa with the theme; “Digital Transformation in public Health practice: Innovations and Impact”.
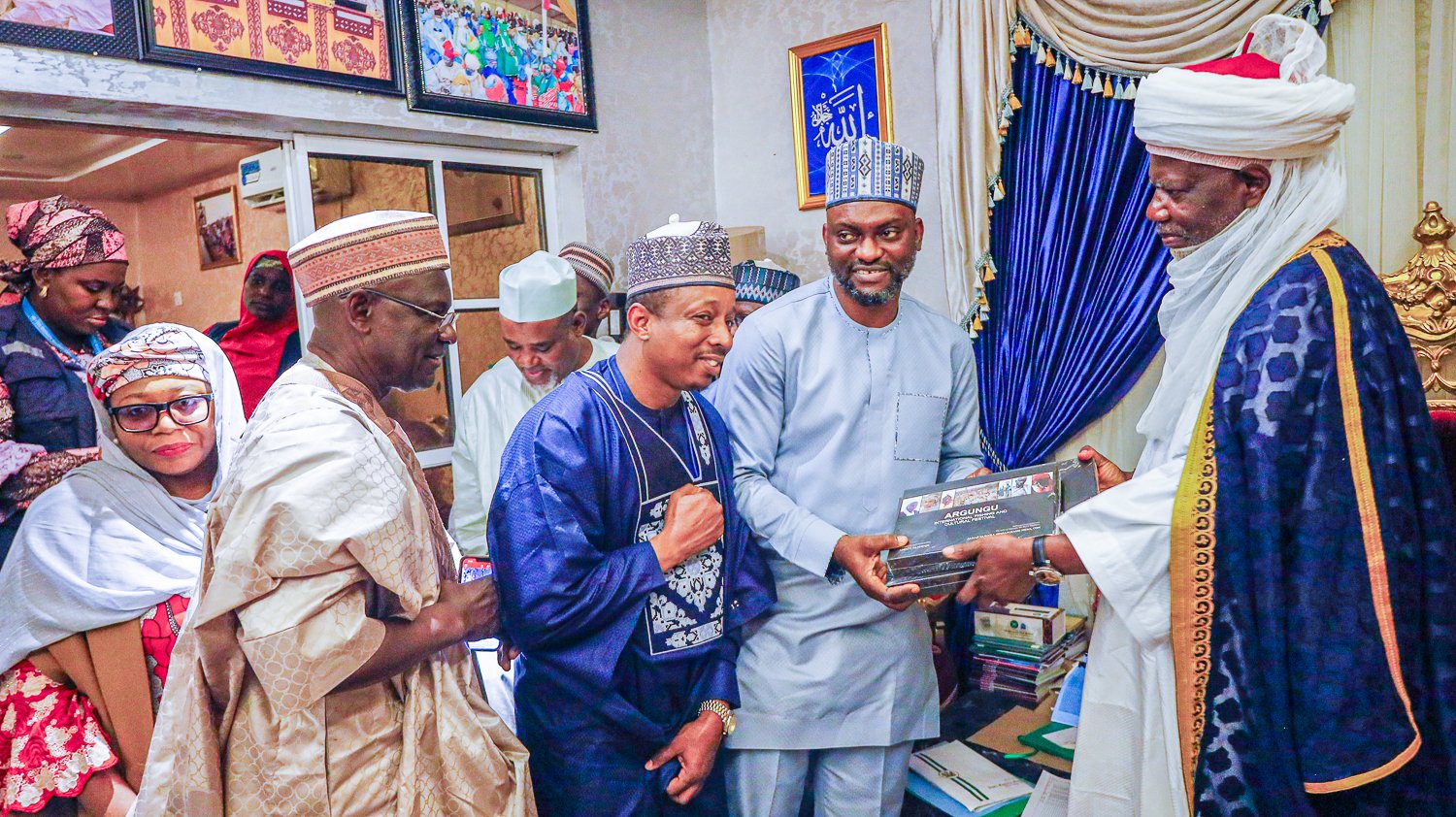
Deputy Director of Partnerships and Programs Dr. David Akpan
Reflecting on the theme of this event, the Deputy Director of Partnerships and Programs Dr. David Akpan raised critical questions on the perceived values and the role of stakeholders in ensuring digital innovation to thrive in public health. He also raised concerns around the investment being made to promote digital innovation and the impact criteria investors are focusing on. He emphasized, “we want to do this because we want to make that grandmother and other persons in the rural community have access to quality healthcare. It's what they call equitable access that removes all barriers”. To achieve this, “you need to do the human-centered design approach, which takes the people into consideration when you're developing any form of innovation”, he stated. Thus he called for the need to document diverse salients points and outcomes from various digital health forums for the purpose of effective advocacy.
eHealth Africa’s Director of Partnerships and Programs Ota Akhigbe
Speaking during the event, eHealth Africa’s Director of Partnerships and Programs Ota Akhigbe said, the event is beyond a conversation on digital innovations but a platform to advocate for a unified approach to digital transformation, emphasizing the importance of integrity in data usage. She revealed that, “The ILF serves as an advocacy tool to raise awareness and engage government agencies, ensuring that these innovations receive the necessary support and funding”. According to Ota, this collaborative approach between the private sector and government agencies is vital for the successful implementation of digital health solutions.
She lauded the positive body language of Government at all levels to support and advance digital innovation in primary healthcare. This, according to her, is why the Insights Learning Forum is an opportunity for the stakeholders to communicate their needs and expectations to government representatives, ensuring that policies are aligned with the sector’s evolving needs.
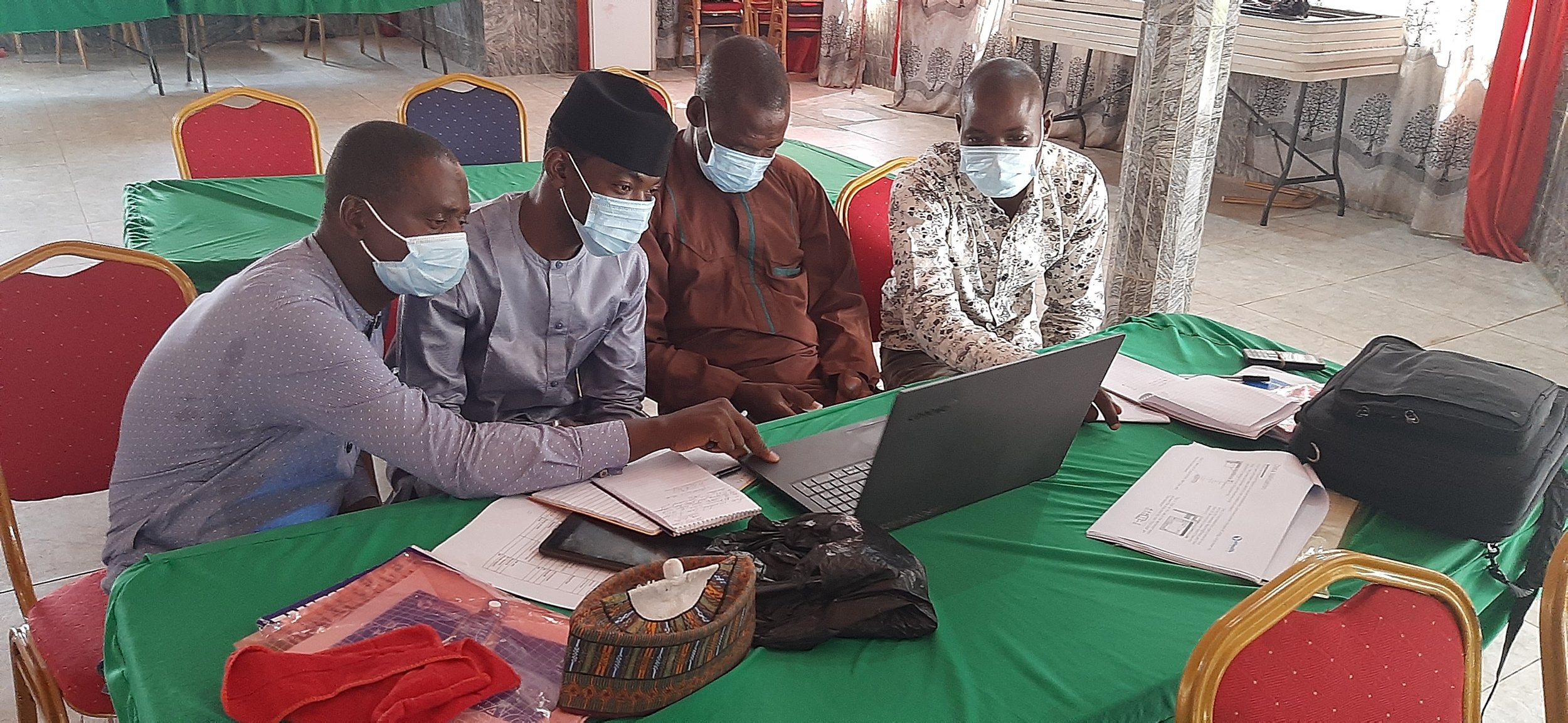
Track Sessions at the IFLF 2024
Speaking on why it's vital for the government to continuously support digital innovations in health sector, Incident Manager, Polio Emergency Operation Center in Katsina state Dr Kabir Sulaiman said, It is very important for us to know that, we need to embrace this era of digital technology that is currently transforming the paper based routine to electronic database. According to the Incident Manager, “Digital innovations will support the strengthening of health systems because some of these digital tools are currently being used in Nigeria.” For instance, “the Surveillance Outbreak Response and Analysis System (SORMAS), which was deployed to the state for reporting priority diseases, has brought about transformation in terms of real-time data and decision-making. So, when you look at the importance, you know there is a lot that we are going to benefit from this technology,” he reiterated.
Through a diverse array of plenary sessions, panel discussions, and track sessions, the Insights Learning Forum 2024, empowered individuals, groups, and organizations to harness digital technologies to address emerging challenges and drive positive change in public health systems in Africa.