By Emmanuel Uko
The journey of supporting and augmenting laboratories in Africa has only started, and evidently, the gap is huge. At the WHO Polio lab in Maiduguri, Borno State, eHA identified cases of damaged, obsolete and inadequate equipment and swung in to supply the needs with support from the World Health Organization (WHO).
As we walked into the office of Professor Marycelin Baba, the Director of the Laboratory, Professor of Medical Virology and lecturer with the University of Maiduguri, we could tell how busy the facility had become on a daily basis. Samples from patients were brought in on a queue for processing. “Our work here is becoming satisfying”, Prof told us expressively, “especially with partnership from the World Health Organization (WHO) and eHealth Africa (eHA). They have provided various major equipment that enable the center to remain functional”, she said, her passion unwavering for 32 years in the profession.
The lab in Maiduguri, was set up by Global Polio Laboratory Network (GPLN), to distinguish poliovirus as a cause of acute flaccid paralysis (AFP) from AFP caused by other diseases. It serves the northern part of Nigeria while the one earlier established in Ibadan, Oyo State, serves the southern part of the country.
Prof. Marycelin Mandu Baba, Director, WHO Polio Laboratory in Maiduguri, is happy to have participated in the polio eradication process in Nigeria.
Photo Credit: eHA
The WHO Polio Laboratory in Maiduguri, like many other labs in developing countries, often grapples with acute shortage of equipment, reagents, machines, power supply and human resource, which affect its productivity. Research has shown that the number of optimally functional laboratories accredited to international standards were 380, as of 2014; 91% of these were in South Africa. This means that 12 out of 49 countries in the region had one or more laboratories accredited to international quality standards; 37 had none. However, the Global Polio Laboratory Network consists of 146 WHO-accredited polio laboratories, in 92 countries, across the six WHO regions of the world.
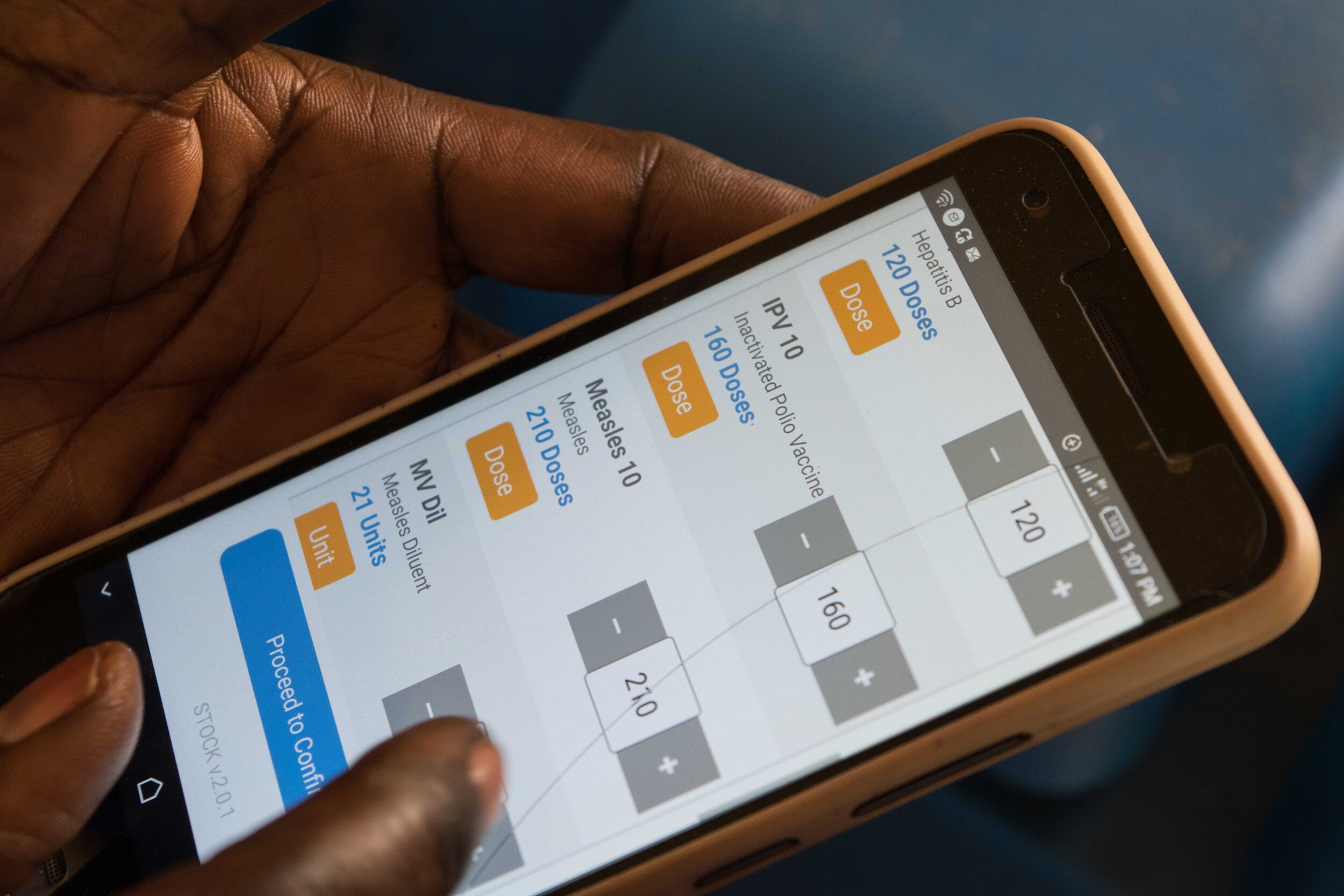
Nigeria has 2 of those 146 WHO-accredited polio laboratories. eHA currently provides support to 7 laboratories: 2 in Nigeria, one each in Uganda, Kenya, Ethiopia, Egypt and the Democratic Republic of Congo. The organization is strategizing to commence support to laboratories in Cameroon, Côte d'Ivoire, Ghana, South Africa, Senegal and Central African Republic. This support will improve laboratory and diagnostic services for Africa’s teeming population. “We continue to carry out needs audits and take steps to offer solutions where we identify gaps,” said eHealth Africa’s Project Manager, Tolulope Oginni. eHA has supported the lab with digitized biosafety cabinets for tissue culture, a Polymerase Chain Reaction (PCR) Workstation, a PCR thermomixer, multi-channel and single-channel pipettes of varied volumes for serology.
Dr Muhammad Talle of the WHO Polio Laboratory in Maiduguri showcases how the new PCR thermomixer donated by eHA works.
Photo Credit: eHA
Dr. Muhammad Talle remains hopeful that the lab will continue to deliver appropriate services according to approved standards.
Photo Credit: eHA
“eHA has brought us relief”, said the Assistant Director for Lab Technical Operations, Dr Bamidele Oderinde, who came in later to the conversation. “The new machines help to reduce technical problems and the functionality complaints we have. We have upgraded our operations, research capabilities and training standards for our students”.
Professor Baba remains keen on contributing her quota towards the eradication of viral diseases, through differential diagnosis of acute flaccid paralysis. According to her, the newly equipped lab benefits people beyond Borno State and extends to other parts of Nigeria. Supporting this lab and other laboratories is part of eHA’s service areas, to build and operate effective laboratories in-country across the globe, and develop the tools and technology needed for effective dissemination and use of public health-related information.
The Director, Prof. Marycelin Baba (3rd right), with eHA delegates and other staff of the laboratory, during eHA’s visit to the lab.
Photo Credit: eHA